
Special bottle-feeding nipples can be employed to bypass the cleft palate and deposit formula to the back of the mouth, where it is more likely to reach the esophagus. 7 Surgical distraction of the mandible, or distraction osteogenesis, eventually can be performed to move the jaw forward and enhance the patency of the airway.įeeding difficulties for infants with Pierre Robin sequence include poor suck due to the presence of a cleft palate, and special care must be taken to ensure adequate caloric intake and growth. Tracheotomy should be reserved for cases in which all other respiratory interventions have failed. If this is not effective or sufficient, continuous positive airway pressure, tongue-lip adhesion, and the use of a nasopharyngeal airway may improve patency. In mild cases, prone positioning alone may be sufficient to maintain patency of the airway by allowing the tongue to move forward and out of the way. 1Ĭomplications stem largely from the infant’s inability to maintain a patent airway or produce a strong suck. Other diagnoses to consider include spondyloepiphyseal dysplasia congenita, Kniest dysplasia, Marshall syndrome, Catel-Manzke syndrome, Toriello Carey syndrome, and Treacher Collins syndrome. It is critical to obtain a genetic consultation when meeting a patient with this triad. Numerous other genetic conditions have been identified that may present with Pierre Robin sequence. Survival rates are very low, and many pregnancies do not reach term. In addition to micrognathia, infants are born with a prominent occiput, microcephaly, low-set ears, and renal and cardiac defects. Trisomy 18 syndrome: Also called Edward syndrome, trisomy 18 is one of the most common trisomies, affecting 1 in 8,000 live births. Velocardiofacial syndrome: This condition, also called DiGeorge syndrome, results from a deletion in band 22q11 and involves congenital heart defects, hypocalcemia and seizures, thymic hypoplasia, and distinctive craniofacial features including mild microcephaly and/or cleft palate. It typically manifests as short stature, campomelia, hearing loss, and scoliosis, in addition to Pierre Robin sequence. 4Ĭampomelic dysplasia: This disorder is due to an autosomal dominant inheritance of the SOX9 gene, leading to a loss of cartilage development. An autosomal dominant mutation is present on the COL2A1, COL11A1, COL11A2, COL9A1, and COL9A2 genes that coding for collagen development. The face may appear flattened due to hypoplasia of the bones of the middle of the face. Stickler syndrome: In addition to glossoptosis, respiratory obstruction, and mandibular hypoplasia, patients with Stickler syndrome have myopia, retinal detachment, hearing loss, and mild short stature. 2 These mutations most commonly are autosomal dominant and associated with collagen development, and they may have other manifestations in addition to craniofacial abnormalities. Pierre Robin sequence can occur as an isolated event from a de novo mutation however, 60% to 80% of cases are associated with known genetic mutations. 2 These craniofacial abnormalities often lead to poor suck and occlusion of the larynx, which may be life-threatening. The ultimate result of this is glossoptosis (the tongue set far back in the mouth) and cleft palate.

#Pierre robin sequence vs treacher collins series
1 It is believed to occur as a result of mandibular hypoplasia initiating a series of events by interfering with placement of the tongue and formation of the palate during prenatal development. Pierre Robin sequence is described as a triad of glossoptosis, mandibular hypoplasia, and cleft palate. The girl received a tentative diagnosis of Pierre Robin sequence pending the results of a workup for a genetic syndrome. Chromosomal microarray analysis was recommended in order to assess whether this variant was pathogenic or benign. The infant struggled to gain weight due to poor feeding secondary to micrognathia, and discharge was delayed until day of life 11, after she had shown adequate weight gain.īlood chromosome analysis revealed a variant on chromosome 20, 46,XX,var(20)(q11.2).
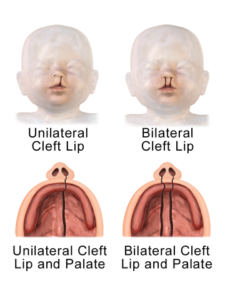
Results of a brain ultrasonogram were normal, and the infant passed her newborn hearing screening test. Family histories were noncontributory, and there is no history of consanguinity. Fetal ultrasonograms showed a small chin but no other abnormalities. There was no history of illness or teratogenic exposure during pregnancy. At birth, the neonate was noted to have micrognathia, cleft palate, pectus excavatum, and metatarsus varus. A 32-year-old gravida 1 mother delivered a girl at 40 weeks’ gestation via normal spontaneous vaginal delivery after an uncomplicated pregnancy.


 0 kommentar(er)
0 kommentar(er)
